Bowel control disorders affect the normal pattern of emptying your bowels. There are many factors that contribute to normal bowel movements, including the consistency of your stools, diet, medical problems, surgical history, ability of the rectum to hold stool and the coordination of various pelvic muscles to allow emptying.
What is normal? That’s hard to say exactly. When it comes to bowels, we are all different. You don’t have to have a bowel movement every day. On average, normal stool frequency is at least 3 bowel movements a week, and no more than 3 stools per day. Stool consistency often varies based on what you’re eating, how much water you drink, and how much exercise you get. The first stop is to pay attention to your OWN normal.
You may want to keep a diary of your bowels to take with you to your doctor’s appointment – chart out the day, time, and consistency of the stools you pass, including any episodes of leakage.
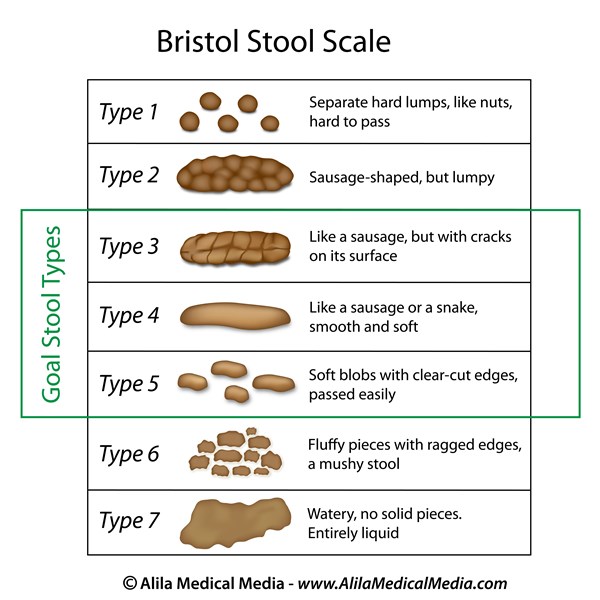
Use this guide to help describe your stools:
Accidental Bowel Leakage
Accidental bowel leakage (ABL), also known as fecal incontinence, is the loss of normal control of the bowels, leading to leakage of solid or liquid stool or gas. About 8 out of every 100 women struggle with ABL. The number of women affected increases with age. And, researchers think that in reality, the total number of women is likely much higher, but many are too embarrassed to seek treatment.
Causes of Accidental Bowel Leakage
There are many causes of accidental bowel leakage, including injury caused during childbirth, damage to the anal sphincter or nerves, pelvic organ prolapse, fistula, medical problems and abnormal stool consistency.
Childbirth Injury
Pregnancy can increase the risk of accidental bowel leakage. It is more common in women who deliver vaginally than women who have a C-section. However, research also suggests that just carrying a pregnancy can increase your risk of these changes as well.
Delivering a large baby vaginally, especially if forceps are used, poses more risk than having a smaller baby. An episiotomy or significant tear of the tissues around the vagina and rectum can result in damage to the nerves, muscles, and tissues around the rectal canal. This can result in a tear of the anal sphincter muscles that help to hold in stool, but also some of the surrounding tissues that are important as well.
Anal Sphincter Injury
There are two main circular muscles, or sphincters, that help to hold in stool near the anal opening. During vaginal childbirth, the anal sphincter muscles can be damaged or torn. These muscles allow us to control bowel movements. It is estimated that as many as 40% of women experience muscle injuries in this area during childbirth. Some of these tears are recognized and repaired, but some are hidden. Injury is more common after episiotomy or forceps delivery.
The anal sphincter muscles can also become weakened for other reasons, such as diabetes or neurologic conditions. They can also be damaged during other surgeries, such as surgery to fix an anal fissure or hemorrhoids. This can cause decreased strength resulting in problems controlling passage of bowel movements.
Ultrasound can help to detect these injuries. Depending on the extent of the injury and the length of time from when it occurred (for example, how long ago you delivered your baby), surgery can repair the damage. If the damage occurred in the past, surgery may not be able to help.
Nerve Injury
Injury to the anal sphincter nerves can cause decreased sensation and muscle strength, both of which can contribute to ABL. Vaginal delivery, chronic constipation, or illnesses that affect the nerves such as diabetes and spinal cord injury can result in nerve damage. For some women, nerve damage that occurs during vaginal delivery improves on its own one or two years after childbirth.
Prolapse
Several types of prolapse can affect bowel control.
-
- Rectocele: A rectocele is a hernia of the bowel upward into the vaginal canal. It causes a vaginal bulge that can sometimes result in difficulty emptying the bowels.
- Rectal prolapse: Rectal prolapse is a condition where the rectum slides out through the anal opening. This causes a bulge coming from the anus, not from the vagina. Distortion of the anal opening can result in damage to the sphincter muscles and bowel leakage.
- Hemorrhoids: Hemorrhoids are caused by enlarged blood vessels near the anal opening. Sometimes they can cause small bulges near the anal opening. These can make it difficult to clean near the anus, resulting in seepage of bowel contents. There are many treatments for hemorrhoids, ranging from medicines to surgery to remove them. However, if hemorrhoids are removed, one out of every 10 women will end up with fecal incontinence.
Fistula
Abnormal openings or connections (tracts or tunnels) known as “fistulas” can develop between the bowel and vagina, or the bowel and the skin. Fistulas can occur:
- After vaginal delivery or vaginal surgery. This is more likely if a large tear occurred during delivery but is still unusual.
- Spontaneously as a result of diverticulitis or other bowel conditions, including Crohn’s disease.
- In patients who have had radiation in the pelvis.
Abnormal Stool Consistency
Bowel movements with normal consistency are easiest to control. Ideally, stools should be like toothpaste. Abnormal stool consistency (either loose or hard stools) may contribute to ABL:
- Diarrhea or loose bowel movements are more difficult to control. This can also increase the sensation of needing to pass stool, called fecal urgency.
- Severe constipation. People who have significant problems passing stool can experience a hard lump of stool with diarrhea that develops around it.
Constipation
Everyone is different, but most women normally have bowel movements at least every other day and no more than twice daily. Having a bowel movement less than three times per week, along with straining to produce a hard bowel movement, is called constipation. Constipation is very common, affecting about 1 in 3 women.
Causes of Constipation
Constipation occurs for several reasons. It may be related to diet or changes in the nerves that control the pelvic floor muscle functioning that can affect the bowels. Lifestyle choices, medicines, or supplements, pelvic floor disorders, lack of exercise, and other health problems may also impact bowel movements.
Dietary Problems
The most common reason for constipation is not having enough fiber in your diet. This is very common in women who eat a typical American diet and getting enough fiber to fix this problem often requires planning and supplementation. The general recommendation is to aim for 25-35 gram/day of fiber between food and supplements.
Some foods, especially those high in starch such as white rice, pasta, or white bread, are more likely to lead to constipation.
Constipation may also be due to lack of fluids in your diet. Some women do not drink enough fluids to keep their stool soft. When there is not enough fiber or water in your diet, bowel movements are more likely to be hard or irregular. However, excessive fluid will not help constipation, especially if there is another underlying dietary problem. Discuss with your provider what the right amount of fluid is for you.
Medicines and Supplements
Talk with your doctor about the medicines and supplements you take, as many can cause constipation. Ask about alternative medicines without constipating effects. Medicines that treat bladder urgency, depression, blood pressure, and pain (especially narcotic medicines) commonly cause constipation. Iron and calcium supplements can do this also.